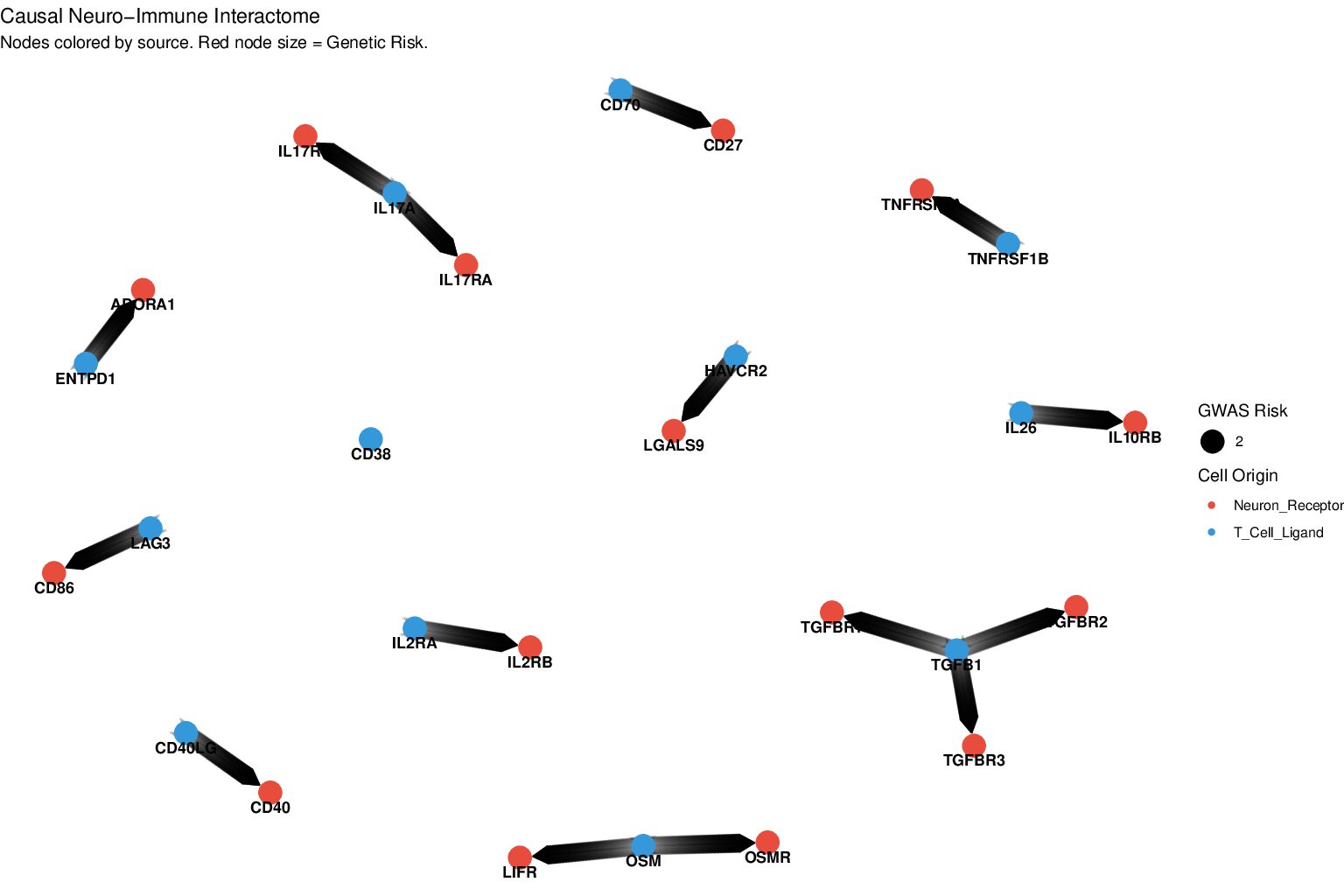
Lewy Body Dementia (LBD) is characterized by the accumulation of alpha-synuclein and chronic neuroinflammation. Despite the identification of risk loci by genome-wide association studies (GWAS), the functional convergence of these genetic factors upon cellular interactions remains largely unmapped. This study hypothesizes that LBD pathogenesis is driven by a genetically primed neuroimmune synapse where antigen-experienced T cells interact with vulnerable neurons. A four-phase computational framework was implemented to integrate multi-omic data, incorporating variant-level signals from LBD GWAS, single-cell RNA and T-cell receptor (TCR) sequencing from cerebrospinal fluid (CSF), and single-nucleus transcriptomics from cortical tissue. Genetic prioritization identified risk genes, including BCAM, GBA, and APOE. Integration with CSF data revealed that these genetic risks converge within clonally expanded Cluster of Differentiation 4 (CD4)+ T cells exhibiting a distinct transcriptional signature marked by upregulation of the cytoskeletal regulator tropomyosin-4 (TPM4) and the lysosomal protease cathepsin H (CTSH). Ligand-receptor modeling identified that these reactive T cells are recruited to Layer 5/6 excitatory neurons via the chemokine ligand 12–C-X-C motif chemokine receptor 4 (CXCL12-CXCR4) and major histocompatibility complex class II (MHC-II) axes. The integrated network demonstrates a molecular convergence where genetic susceptibility to LBD is manifested through a cytotoxic, lysosomal-enriched T cell response targeting vulnerable cortical neurons. This provides a structural basis for the neuroimmune synapse in LBD and suggests new avenues for immunomodulatory intervention.
Decoding the Neuroimmune Synapse in Lewy Body Dementia: Genetic risk convergence on CD4⁺ T cell–neuron interactions